Case Management/Utilization Management/Denial Management
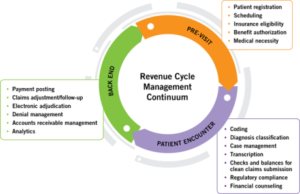 Quality Healthcare Partners (Quality) offers consulting services to organizations that are interested in improving their case management (CM), utilization review (UR), and denial management (DM) processes with specific emphasis on medical necessity admission, continued stay, and denial management. CM/UR/DM programs are evolving with the move toward value-based care, bundled payments and risk sharing contracts. Now is the time for a check-up to see if your operational model is achieving the desired outcomes and is aligned optimally with your revenue cycle. In the last decade CM and UR functions were merged into one, but now with cash flow critical to an organization’s success, it is imperative to re-examine workflows and processes to identify what is working and what is not. A third-party audit of your CM/UR/DM activities and their interactions with revenue cycle management (RCM) can be valuable in making measurable improvements and proactively decreasing length of stay, denials and readmissions.
Quality Healthcare Partners (Quality) offers consulting services to organizations that are interested in improving their case management (CM), utilization review (UR), and denial management (DM) processes with specific emphasis on medical necessity admission, continued stay, and denial management. CM/UR/DM programs are evolving with the move toward value-based care, bundled payments and risk sharing contracts. Now is the time for a check-up to see if your operational model is achieving the desired outcomes and is aligned optimally with your revenue cycle. In the last decade CM and UR functions were merged into one, but now with cash flow critical to an organization’s success, it is imperative to re-examine workflows and processes to identify what is working and what is not. A third-party audit of your CM/UR/DM activities and their interactions with revenue cycle management (RCM) can be valuable in making measurable improvements and proactively decreasing length of stay, denials and readmissions.
Who Can Benefit from Quality’s CM/UR/DM Consultative Services?
- Rural hospitals
- Hospital systems
- Clinical integrated healthcare systems
- Academic medical centers
- Health plans and the health insurance marketplace
- Accountable Care Organizations (ACOs)
- Centralized UR departments
- Utilization management and case management companies
- Community and regional hospitals
Our Experience and Service Offerings
Quality’s executive-level consultants specialize in organizational transformations. Their credentials include the actual management of case management, utilization review and denial management and the development of programs that are aligned with revenue cycle management. As part of our services, we provide a comprehensive needs assessment, gap analysis and detailed action plans to achieve a more cohesive interaction among the respective departments. Quality’s consulting services will optimize your organizational operations so that they can effectively respond to the demands of bundled payments, Medicare readmission penalties and effective progression of care.
What We Offer as Part of Our CM/UM/DM Evaluation Services
Quality’s experts will perform an onsite assessment of your organization’s operational processes and will provide you with a detailed report of its findings, conclusions and recommendations. In performing our analyses, we will observe work flows, collect data, and will utilize sophisticated analysis techniques such as:
- Strength, weaknesses, opportunities and threats (SWOT) assessment
- Value stream analysis
- Performance baselining and benchmarking
- Rapid process improvement workshops
- Root cause determinations.
Our recommendations will identify specific opportunities for improvement in such areas as:
- Organizational structure and leadership
- Operational priorities and time lines for organizational change
- UR/CM models best for your setting
- Areas to improve alignment with Revenue Cycle Management
- Payer mix and payer-driven methodologies for authorization and re-authorization
- Barriers to progressive care and solutions
- Assessment of UR and transition of care skills of case managers
- Documentation quality
- Appropriateness of admissions including the two-midnight rule processes/documentation
- Evaluation of Emergency Departments and the planned admission processes
- Patient documentation – estimated time patient will require hospitalization, continued medical necessity
- Adequacy of tools and the education needs of case management staff
- Training and orientation curriculum
- Determination of readmission rates and length of stay
- Review missed opportunities to convert observation stays to in-patient stays
- Evaluation of the initial 24-hour level of care assessments performed and patients/families’ expectations for admission/discharge
- On-Site UR/CM Model Implementation Support
- Webinar and Onsite Education Training
- Future Design Case Management Model Development
- On-Site Interim Case Management Director Support
Clinically Focused Revenue Cycle Action Planning
It has never been more critical for the financial stability of hospitals and health care systems to implement sustainable clinically focused revenue programs that interface with case management, admitting, clinical documentation and chart capture. As part of our service offering, Quality can also provide a team of revenue cycle experts that can implement specific programs such as mandatory bundled payment, analyze and improve revenue cycle process and develop training curriculum. For example, Quality could provide seasoned veterans for one or more of the following roles:
- Interim Utilization Management Director
- Interim Case Management Director
- Interim Senior Financial and Accounts Receivable Analyst
- Interim Business Office Director Support
- Interim Revenue Cycle Director Support
- Interim Patient Financial Services Director Support
- Interim HIPAA Security or Privacy Director/Manager Support
- Interim CFO Support
- Interim ACO Population Health Director Support
- Interim Health Plan Support
- Interim Technical Revenue Cycle Business Analyst
- Interim Staffing for software design, testing, integration and implementation
Benefits to Your Organization
- Avoid painful, expensive mistakes, problems, and surprises
- Obtain third party independent audit recommendations
- Improve organizational efficiency and productivity tailored to your organization
- Learn from others who have successfully accomplished CM/UR/RCM Department implementations
- Address organizational and resource concerns by bringing objective and experienced expertise to work side by side with your people
- Implement appropriate work process changes that meet your business initiatives and goals
